SUD Patients Lean on Mobile Recovery Apps During COVID-19 as Opioid-Related Overdose Cases Spike
August 26, 2020
By Hans Morefield, CEO, CHESS Health
Social isolation is hard on most people, but for those living with Substance Use Disorder (SUD), it can be deadly. Suspected opioid overdoses rose 18% in March, 29% in April, and 42% in May.[1] Being around peers and family help patients feel connected and supported—both essential for a successful recovery. But with COVID-19, in-person AA meetings and other support groups have been cancelled or have moved online. While a virtual meeting is better than no meeting at all, it lacks the intimacy of an in-person group and makes communication among the group more challenging. This can lead to depression and anxiety, which can fuel relapse.
Counselors and therapists, too, have moved from in-person appointments to telehealth. Again, while this approach is better than no appointment, it, too, comes with many challenges. Patients who live within close quarters to others may find it difficult to find privacy during a video call, which means they may not be fully forthcoming with the counselor for fear of being overheard. Telehealth also removes the ability to drug test or screen patients for signs of abuse prior to an appointment.
Another factor that has led to increasing opioid deaths during COVID is the interruption in the drug supply chain, which has led many dealers to use synthetic and potentially lethal substances as a replacement.[2] For patients who’ve been through detox, taking the same dose they were previously accustomed to—whether “pure” or not—the result is more likely to be overdose and death.
Removing the Isolation Barrier

One way healthcare professionals are mitigating these risks is through mobile recovery apps that keep patients connected with their peers, clinicians, and families in a way that remains private and is always available.
How CHESS Health Supports Recovery
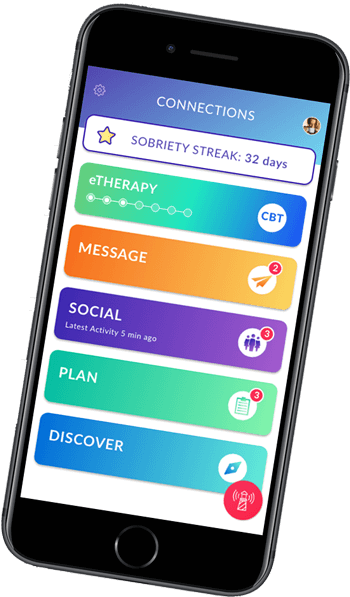
The Connections App from CHESS Health is one example, of a company providing patients with the tools they need right in the palm of their hands The Connections App provides multiple support features, including: anonymous group messaging with peers, sobriety tracking, daily surveys, recovery tracking, educational and motivational content, and crisis line access. Connections also includes a companion app that helps clinicians engage with patients, while tracking and analyzing their progress. Having this tool helps clinicians provide more informed, personal, and effective support to their patients.
Research shows that patients who use these tools are more likely to keep appointments, adhere to care plans, attend more treatment days, and they are more motivated to stick with their programs.[3] Research on the Connections App also shows a lower likelihood of relapse.[4]
There’s No Time to Wait
The latest statistics are proof of the devastation this pandemic is having on those living with SUD. Unfortunately, relief efforts have failed to adequately address this issue. Of the $2.5 trillion in relief funds, only $425 million has been allocated for mental health and SUD treatment. As the Washington Post points out, this is “barely more than a hundredth of one percent.”[5] In other words, SUD providers and organizations are going to have to look for innovative ways to help patients make it through this difficult time. And it’s critical that we act soon as some healthcare experts are warning that COVID-19, or some version of it, may be with us for years.[6]
We’ve already gotten a small glimpse of the challenges we face during this pandemic. It is, unfortunately, a learn-as-we-go scenario. But that’s not the case when it comes to treating patients with SUD. We know the risks they’re facing and we have proven technology to help reduce the impact of isolation. The situation at hand is dire and we must do all we can now to keep the scourge of overdose from becoming the next pandemic.
[1] https://www.washingtonpost.com/health/2020/07/01/coronavirus-drug-overdose/
[2] ibid.
[3] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3419880/
[4] Published studies available at www.chess.health/evidence
[5] https://www.washingtonpost.com/health/2020/07/01/coronavirus-drug-overdose/
[6] https://science.sciencemag.org/content/368/6493/860.full
